- Introduction
India has emerged as the global epicenter of diabetes, now holding the highest number of cases worldwide, with an alarming estimate of 212 million adults affected. This figure surpasses that of China, which reports 148 million cases, as highlighted in recent studies published in The Lancet and other scholarly sources. These statistics underscore the rapid growth of diabetes as a critical public health challenge, particularly in low- and middle-income countries.
Globally, diabetes affects over 400 million individuals, with South Asia being a significant contributor to this epidemic. In India, diabetes prevalence has escalated due to urbanization, sedentary lifestyles, and dietary shifts. Recent pooled data from global health studies reveal that the prevalence rate of diabetes in India ranges from 11% to 15%, reflecting a substantial burden on healthcare systems. This crisis is compounded by the rising incidence of prediabetes, with nearly 25 million Indians at high risk of developing the condition, potentially inflating the future diabetes population further.
The gravity of the situation extends beyond sheer numbers, as the economic and healthcare implications of managing diabetes-related complications, including cardiovascular diseases, kidney failure, and neuropathy, are immense. With these statistics signaling a dire need for immediate action, India faces the dual challenge of implementing preventive strategies while managing an already vast diabetic population.
This introduction provides a foundation to explore the multifaceted dimensions of diabetes in India, including its causes, implications, and potential strategies for control and mitigation.
2. Background
Defining Diabetes (Type 1 and Type 2) and Its Health Implications
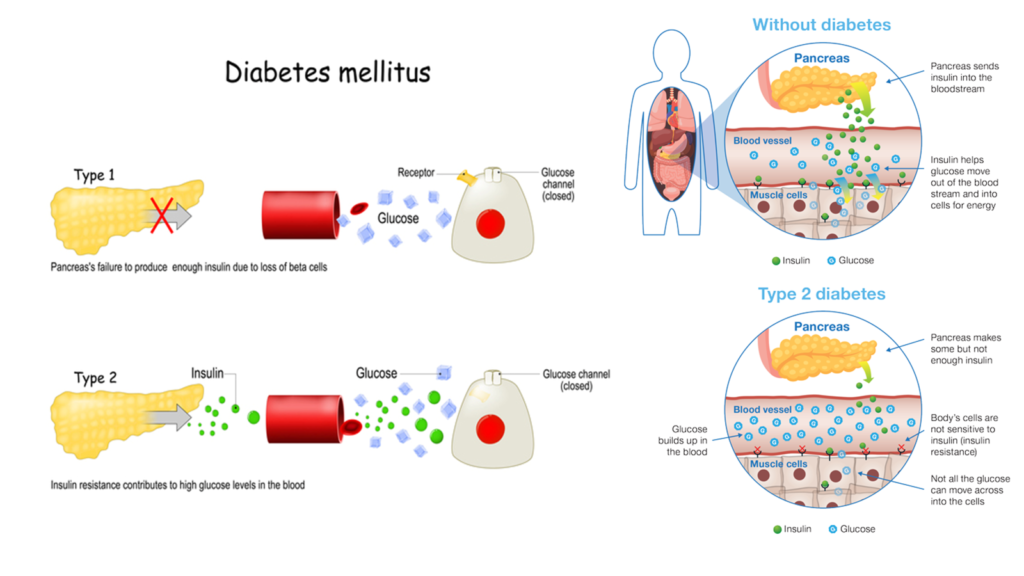
Diabetes mellitus is a chronic metabolic disorder characterized by elevated blood glucose levels, either due to insufficient insulin production or ineffective insulin utilization by the body. The condition primarily exists in two forms:
- Type 1 Diabetes: An autoimmune disorder in which the immune system attacks insulin-producing beta cells in the pancreas. This form accounts for approximately 5-10% of all diabetes cases and typically manifests in childhood or adolescence. Without insulin therapy, individuals with Type 1 diabetes face life-threatening complications.
- Type 2 Diabetes: The more common form, Type 2 diabetes, results from insulin resistance and inadequate compensatory insulin secretion. Often associated with obesity, sedentary lifestyles, and genetic predisposition, Type 2 diabetes accounts for over 90% of global diabetes cases. It typically develops in adulthood but is increasingly being diagnosed in younger populations due to rising childhood obesity.
Health Implications: Diabetes leads to numerous complications, both acute and chronic, including:
- Cardiovascular Complications: People with diabetes are at significantly higher risk of heart disease, stroke, and hypertension.
- Kidney Damage (Nephropathy): Persistent high glucose levels can damage the kidneys, often leading to kidney failure.
- Eye Disorders (Retinopathy): Diabetes is a leading cause of blindness due to retinal damage.
- Nerve Damage (Neuropathy): Peripheral neuropathy can cause pain, tingling, or loss of sensation, often leading to injuries and infections in extremities.
- Amputations: Untreated wounds and infections can result in amputations, particularly of the feet.
- Mental Health Impact: Diabetes is linked to increased rates of depression and anxiety due to the chronic nature of the disease and its management demands.
Exploring Global Trends in Diabetes Prevalence
Diabetes prevalence has increased dramatically worldwide in recent decades. According to the International Diabetes Federation (IDF), over 537 million adults (20-79 years) were living with diabetes in 2021, and this number is projected to reach 783 million by 2045. Factors contributing to this surge include rapid urbanization, unhealthy dietary practices, obesity, aging populations, and genetic predispositions in certain ethnic groups.
Key Global Trends:
- Rising Burden in Low- and Middle-Income Countries: Over 75% of people with diabetes live in low- and middle-income countries. These regions face the dual burden of managing infectious diseases and increasing non-communicable diseases like diabetes.
- Childhood Obesity and Early Onset: The global rise in childhood obesity has led to earlier onset of Type 2 diabetes, a condition once considered rare in children.
- Urbanization and Sedentary Lifestyles: Urban living environments promote sedentary behaviors and easy access to calorie-dense processed foods, exacerbating diabetes risk.
- Healthcare Inequities: Limited access to affordable care, particularly in resource-constrained settings, has resulted in high rates of undiagnosed diabetes and poorly managed cases, further complicating outcomes.
Importance of Monitoring Diabetes in Populous Countries like India and China
India and China together account for a significant portion of the global diabetes burden due to their large populations, rapid socioeconomic changes, and genetic predispositions. Key factors making monitoring essential in these countries include:
- Scale of the Problem:
- India: With an estimated 212 million diabetes cases, India is now the global leader in diabetes prevalence.
- China: Following closely, China has 148 million cases, making it the second-largest contributor to the global diabetes epidemic.
- Socioeconomic Implications:
- The economic burden of diabetes management, including healthcare costs and lost productivity, is immense in these nations. For example, direct healthcare costs for diabetes treatment exceed billions annually in both countries.
- Out-of-pocket expenses, particularly in rural and underprivileged areas, exacerbate financial stress on families.
- Intergenerational Impact:
- Diabetes during pregnancy (gestational diabetes) is increasingly common in India and China, affecting fetal health and increasing the likelihood of diabetes in the next generation.
- Public Health Challenges:
- With a high percentage of undiagnosed cases, large-scale screening programs are necessary.
- Insufficient infrastructure for chronic disease management in rural areas makes early diagnosis and consistent treatment challenging.
- Learning from Global Best Practices:
- Both nations can benefit from global strategies like improved healthcare access, community-based interventions, and promoting awareness through public health campaigns.
3. Key Findings from the Report
India Overtaking China in Diabetes Numbers
Recent data indicates that India has surpassed China to become the global leader in diabetes prevalence, with an estimated 212 million cases compared to China’s 148 million. This shift highlights the scale of the diabetes epidemic in India, where socioeconomic transformations and lifestyle changes have driven an unprecedented rise in cases. While China once dominated global diabetes statistics, rapid urbanization and lifestyle alterations in India have led to a steeper trajectory in diabetes prevalence, making it a critical public health issue.
Factors Contributing to the Rise
- Lifestyle Changes:
- Increased consumption of calorie-dense and processed foods, particularly in urban areas, has contributed to rising obesity and diabetes rates.
- Sedentary behaviors, including reduced physical activity due to desk jobs and digital entertainment, have exacerbated the problem.
- Unhealthy eating patterns, including high carbohydrate intake and low dietary fiber, are common contributors.
- Urbanization:
- Urban living promotes lifestyles associated with diabetes, such as reduced physical activity, reliance on motorized transportation, and limited green spaces for exercise.
- Urban areas in India have better access to diagnostic facilities, which may also partially explain the higher detection rates compared to rural regions.
- Genetic Predisposition:
- South Asians have a genetic predisposition to insulin resistance, even at lower body mass indices, making them more vulnerable to Type 2 diabetes.
- Studies suggest that individuals of Indian origin develop diabetes a decade earlier than their Western counterparts, often with severe complications.
- Socioeconomic Factors:
- Economic growth has led to shifts in dietary habits and decreased physical labor, both of which contribute to diabetes.
- Widespread economic disparities mean that many individuals are unable to afford proper treatment or lifestyle modifications, leading to poorer health outcomes.
Related Health Challenges
- Obesity:
- India is experiencing a parallel rise in obesity, with rates reaching epidemic proportions, particularly in urban areas. Obesity is a major risk factor for Type 2 diabetes and worsens disease prognosis.
- Abdominal obesity, characterized by high visceral fat, is especially prevalent among Indians, further increasing their susceptibility to diabetes.
- Hypertension:
- Hypertension affects nearly one in three Indian adults and often coexists with diabetes, compounding the risk of cardiovascular complications.
- Studies indicate that hypertensive individuals with diabetes have a significantly higher risk of heart attack, stroke, and kidney disease.
- Cardiovascular Disease:
- The coexistence of diabetes, obesity, and hypertension contributes to an accelerated risk of cardiovascular diseases, which remain the leading cause of death in India.
- Kidney Disease:
- Diabetic nephropathy, or kidney damage caused by prolonged high blood sugar levels, is on the rise. Without early detection and management, many patients progress to end-stage kidney disease requiring dialysis or transplantation.
- Mental Health Impact:
- The chronic nature of diabetes and its complications can lead to anxiety, depression, and psychological distress, further reducing quality of life.
4. Contributing Factors in India
India’s status as the country with the highest number of diabetes cases globally is driven by several interlinked factors. These contributing elements have both behavioral and systemic origins, compounded by rapid socioeconomic changes.
Sedentary Lifestyles and Dietary Shifts
- Decreased Physical Activity:
- Urbanization has led to a significant decline in physical activity levels, with many individuals transitioning from physically demanding jobs in agriculture and labor to sedentary office jobs.
- Increased use of motorized transportation and limited recreational infrastructure in cities further discourage active lifestyles.
- Unhealthy Diets:
- Dietary patterns have shifted from traditional high-fiber, low-calorie diets to diets rich in refined carbohydrates, unhealthy fats, and sugars.
- The proliferation of fast food and processed snacks has exacerbated poor dietary habits, particularly among urban youth.
- Snacking Culture:
- The growing popularity of sugar-laden snacks and beverages, especially among children and teenagers, contributes to obesity and insulin resistance.
Urbanization and Increased Access to Unhealthy Food Options
- Rapid Urbanization:
- Urbanization has transformed dietary and physical activity patterns. Access to high-calorie foods and sedentary occupations dominate urban lifestyles.
- Urban populations experience higher stress levels, often resulting in stress-related overeating and metabolic disturbances.
- Food Environment:
- Supermarkets, fast-food chains, and convenience stores have made calorie-dense, nutrient-poor foods more accessible and affordable, displacing traditional and healthier dietary choices.
- Pollution and Lack of Green Spaces:
- Air pollution in urban areas has been linked to metabolic changes and a higher risk of Type 2 diabetes.
- The absence of safe and accessible green spaces discourages outdoor exercise.
Awareness and Diagnosis Improvements
- Increased Detection:
- Advances in healthcare infrastructure, particularly in urban centers, have led to higher rates of diagnosis. Many cases that previously went undetected are now being identified.
- Screening initiatives by the government and private organizations have improved detection rates, though rural and underserved populations remain less reached.
- Health Campaigns:
- Public health campaigns and growing media coverage have raised awareness about diabetes symptoms and complications.
- Social media platforms are increasingly being used to disseminate information, encouraging individuals to seek medical advice early.
- Technological Advancements:
- Technology-driven initiatives, including mobile apps and telemedicine, have enabled better access to diagnostic services and management tools, albeit primarily in urban and semi-urban areas.
Socioeconomic Disparities and Health Literacy Issues
- Economic Inequality:
- A stark divide exists between urban and rural areas in terms of access to healthcare, nutritious food, and physical activity resources. Lower-income groups often rely on cheap, calorie-dense foods, increasing their diabetes risk.
- For many families, the high cost of managing diabetes, including medications, consultations, and tests, poses a significant financial burden.
- Health Literacy:
- Low health literacy rates, particularly in rural areas, result in a poor understanding of diabetes risk factors, symptoms, and management strategies.
- Misinformation about diabetes treatment, such as reliance on unverified alternative remedies, further hinders effective management.
- Cultural and Social Barriers:
- In some regions, diabetes is stigmatized, leading to delays in seeking diagnosis and treatment.
- Gender disparities in healthcare access mean that women, particularly in rural areas, often have undiagnosed and untreated diabetes.
5. Public Health Implications
India’s unprecedented diabetes epidemic carries significant public health implications, affecting healthcare systems, economic stability, and individual well-being. This multifaceted crisis poses challenges that demand immediate and coordinated action.
Growing Burden on Healthcare Infrastructure
- Increased Demand for Healthcare Services:
- The sheer volume of diabetes cases places immense pressure on healthcare infrastructure, particularly in urban centers where diagnostic and treatment facilities are concentrated.
- The management of diabetes requires continuous monitoring, laboratory testing, and specialized care, which strains existing healthcare resources.
- Inadequate Access in Rural Areas:
- While urban centers have relatively better healthcare access, rural areas lack adequate diagnostic tools, trained healthcare professionals, and treatment facilities.
- Late diagnosis and poor management in these regions lead to higher rates of complications, increasing the need for tertiary care services.
- Overburdened Hospitals:
- The rise in diabetes-related complications, such as cardiovascular events and kidney failure, contributes to higher hospitalization rates, overwhelming hospitals already stretched by other non-communicable and infectious diseases.
- Shortage of Specialists:
- There is a shortage of endocrinologists, diabetologists, and trained primary care physicians equipped to manage the growing diabetic population effectively.
Economic Impact of Diabetes Treatment and Complications
- Direct Medical Costs:
- Diabetes management is expensive, involving costs for medications, glucose monitoring devices, insulin therapy, and regular check-ups.
- The annual cost of diabetes treatment for the average Indian household can consume a significant portion of their income, with poorer families disproportionately affected.
- Indirect Costs:
- Diabetes reduces productivity due to missed workdays, disability, and premature mortality, impacting household income and national economic growth.
- Caring for diabetes-related complications such as amputations, blindness, and chronic kidney disease adds to the economic burden.
- National Economic Burden:
- The cumulative economic impact of diabetes in India runs into billions annually, factoring in healthcare expenses and loss of productivity.
- Studies suggest that non-communicable diseases, including diabetes, will contribute significantly to economic losses in low- and middle-income countries like India by 2030.
- Out-of-Pocket Expenditures:
- With limited insurance coverage, most diabetes-related healthcare expenses are borne out-of-pocket, pushing many families into financial distress.
Potential Rise in Diabetes-Related Diseases
- Cardiovascular Disorders:
- Diabetes significantly increases the risk of heart disease and stroke. Studies indicate that individuals with diabetes are two to four times more likely to develop cardiovascular disorders.
- Cardiovascular diseases remain the leading cause of death among diabetics, requiring extensive and costly medical interventions.
- Kidney Failure (Diabetic Nephropathy):
- Prolonged high blood sugar levels damage the kidneys, leading to diabetic nephropathy. India already sees a rising number of patients requiring dialysis or kidney transplants, which are resource-intensive treatments.
- Blindness and Vision Impairment:
- Diabetic retinopathy is a leading cause of vision loss and blindness in India. Early detection and treatment can mitigate progression, but awareness and access to care remain insufficient in many areas.
- Neurological Complications:
- Peripheral neuropathy caused by diabetes leads to pain, tingling, and loss of sensation in the limbs. Severe cases result in injuries, ulcers, and amputations.
- Autonomic neuropathy affects vital functions, including digestion, blood pressure regulation, and heart rate.
- Infectious Diseases:
- Diabetes weakens the immune system, increasing vulnerability to infections such as tuberculosis, urinary tract infections, and skin conditions.
- During the COVID-19 pandemic, individuals with diabetes faced higher risks of severe complications and mortality.
6. Prevention and Mitigation Strategies
The rapid rise in diabetes prevalence in India necessitates comprehensive and multi-pronged prevention and mitigation strategies. These efforts must target systemic, behavioral, and societal factors contributing to the epidemic.
Government Initiatives to Combat Diabetes
- National Programs:
- The Indian government launched the National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases, and Stroke (NPCDCS), which focuses on early diagnosis, prevention, and management of non-communicable diseases, including diabetes.
- Programs such as the Ayushman Bharat Yojana aim to improve healthcare access and reduce the financial burden on low-income families.
- Awareness Campaigns:
- Campaigns like “Fit India Movement” promote physical activity and healthy lifestyles.
- Government-supported media campaigns increase awareness of diabetes symptoms, complications, and preventive measures.
- Policy Measures:
- Introduction of taxes on sugar-sweetened beverages and subsidies for healthy foods aim to influence dietary behaviors.
- Urban planning policies encourage the creation of green spaces for physical activity.
- Community-Level Initiatives:
- Public health programs at the community level involve healthcare workers in rural areas to screen for and monitor diabetes and provide health education.
- Integration of traditional medicine, including yoga and Ayurveda, into diabetes prevention programs.

The Role of Lifestyle Changes: Diet, Exercise, and Stress Management
- Dietary Modifications:
- Reducing consumption of processed foods, sugary beverages, and refined carbohydrates while promoting whole grains, vegetables, and lean proteins is crucial.
- Nutritional education campaigns can encourage healthy eating habits, especially among youth and families.
- Regular Exercise:
- Moderate physical activity, such as walking, cycling, or yoga, can significantly reduce diabetes risk and help manage blood glucose levels in diagnosed individuals.
- Corporate wellness programs and incentives for gym memberships are strategies to promote fitness among working professionals.
- Stress Management:
- Stress is a known contributor to insulin resistance and poor glycemic control. Practices such as mindfulness, meditation, and breathing exercises are effective in managing stress levels.
- Workplace initiatives to reduce burnout and promote mental health can have a positive impact.
Importance of Early Detection and Education Programs
- Early Screening:
- Widespread screening programs, especially in high-risk populations such as urban dwellers and individuals with a family history of diabetes, can identify cases early.
- Portable diagnostic tools and telemedicine initiatives are helping to bridge the gap in remote and rural areas.
- Health Education:
- Community-based education programs help improve health literacy, empowering individuals to make informed decisions about their diet, physical activity, and healthcare.
- Schools and colleges are vital platforms for instilling lifelong healthy habits in young people.
- Technological Support:
- Mobile apps for diabetes management and awareness provide users with personalized guidance on diet, exercise, and medication adherence.
- Wearable health devices for glucose monitoring enable early detection and proactive management of diabetes.
Collaboration Between Public and Private Healthcare Sectors
- Public-Private Partnerships (PPPs):
- Collaborative efforts between government agencies and private healthcare providers can improve access to diabetes care. For instance, PPPs can enhance the reach of affordable diagnostic services and specialized treatments.
- Leveraging private sector innovation in telemedicine and diagnostics can bring cost-effective solutions to underserved areas.
- Pharmaceutical Industry Engagement:
- Partnerships with pharmaceutical companies to subsidize medications and insulin therapies can make treatment more accessible.
- Research collaborations focus on developing India-specific solutions, such as cost-effective generic drugs and advanced treatment modalities.
- Corporate Social Responsibility (CSR) Programs:
- Private companies can fund diabetes awareness drives, wellness programs, and infrastructure development in underprivileged areas under CSR initiatives.
- Integrated Care Models:
- Multi-disciplinary care involving endocrinologists, dieticians, psychologists, and social workers provides comprehensive diabetes management.
- Establishing community diabetes clinics in collaboration with private players can improve localized care delivery.
7. Global Comparisons and Lessons
How China and Other Countries Are Addressing Diabetes
- China:
- Integrated Healthcare System: China has leveraged its vast network of community healthcare centers to implement diabetes screening, education, and management at the grassroots level.
- Digital Health Solutions: Programs like mobile apps and telemedicine platforms enable remote monitoring and consultation, addressing the needs of its rural population.
- Government Policies: China’s National Health Commission has established guidelines to encourage regular physical activity, improve diet, and reduce obesity.
- Workplace Wellness Programs: Employers are encouraged to promote physical activity and provide healthy meal options to reduce diabetes risks among employees.
- United States:
- Comprehensive Care Models: The U.S. employs patient-centered medical homes (PCMHs) that offer multi-disciplinary care, including specialists, dieticians, and mental health counselors, for holistic diabetes management.
- Insurance Coverage: Insurance programs, such as Medicaid and Medicare, provide subsidized or free care to low-income and elderly populations.
- Behavioral Interventions: Community programs, like the Diabetes Prevention Program (DPP), focus on lifestyle changes and have shown measurable success in reducing Type 2 diabetes onset.
- European Union:
- Preventive Policies: Countries like Finland have implemented national diabetes prevention programs targeting lifestyle changes through structured counseling.
- Sugar Taxation: Several European nations, including the UK and France, have introduced sugar taxes to discourage consumption of sugary beverages.
- Public Education Campaigns: Awareness programs and clear nutritional labeling are used to empower individuals to make healthier choices.
- Australia:
- Data-Driven Strategies: Nationwide registries track diabetes prevalence, enabling targeted interventions.
- Focus on Indigenous Communities: Tailored programs address diabetes risk factors specific to indigenous populations, who face higher prevalence rates.
Lessons India Can Learn from Global Best Practices
- Strengthening Primary Healthcare:
- Develop a robust network of primary healthcare centers similar to China’s model for early screening and management of diabetes in underserved areas.
- Promoting Technology Integration:
- Adopt scalable digital health solutions, such as mobile apps for diabetes self-management and telemedicine platforms to extend care to rural areas.
- Policy-Level Changes:
- Introduce taxes on sugar-sweetened beverages and unhealthy foods while subsidizing healthy alternatives, as done in Europe.
- Regulate food labeling to promote transparency and inform healthier choices.
- Behavioral Intervention Programs:
- Establish structured programs similar to the DPP in the U.S., focusing on lifestyle changes to prevent diabetes onset in high-risk populations.
- Incentivizing Preventive Care:
- Provide incentives, such as insurance discounts, for individuals who maintain a healthy lifestyle and achieve measurable health goals.
- Community-Specific Strategies:
- Learn from Australia’s approach by creating culturally sensitive interventions to target high-risk communities, such as rural and tribal populations.
- Building Collaborative Care Models:
- Integrate multi-disciplinary care involving endocrinologists, dieticians, and psychologists into diabetes management programs, ensuring comprehensive treatment.
8. Conclusion
Recap the Significance of the Issue
India’s emergence as the global leader in diabetes cases is a significant public health concern, with over 212 million individuals affected. The rapid rise in prevalence is attributed to lifestyle changes, urbanization, genetic predisposition, and socioeconomic disparities. The associated burden on healthcare systems, the economy, and individual well-being is immense, demanding immediate attention.
Urge for Immediate and Collaborative Action
To tackle this epidemic, India must adopt a multi-faceted approach involving:
- Government-led policy reforms and prevention programs.
- Public-private partnerships to improve healthcare accessibility and affordability.
- Community-based initiatives to promote awareness and early detection.
- Individual behavioral changes focusing on diet, exercise, and stress management.
End with a Call to Focus on Preventive Healthcare
Prevention must be the cornerstone of India’s diabetes strategy. By prioritizing public health interventions, lifestyle education, and community participation, India can curb the rising tide of diabetes and its complications. Collaborative action from policymakers, healthcare providers, and citizens is essential to create a healthier, diabetes-free future.